Did you get a sense of unhappiness or discontent in elderly relatives when you last saw them? It might be easy to write this off as a bad day, but it could be possible that the person is experiencing a more pronounced depression that they might struggle to communicate clearly. Recognizing Depression in Older People
Depression in older people can often go unnoticed, either through failing to recognize it or the senior citizen doing their utmost to conceal it. Keeping it bottled up is the worst thing to do; if you spot an elderly relative who seems unhappy, talk to them about it. That could be the conversation they crave and, in knowing that someone truly cares, their depression might ease considerably, if not disappear entirely.


Thanks to Be Independent Home Care for supplying this helpful infographic on how to recognize signs of depression in older people and what you can do to help seniors who are experiencing depression.
Recognizing Depression in Older People Recognizing Depression in Older People Recognizing Depression in Older People Recognizing Depression in Older People Recognizing Depression in Older People Recognizing Depression in Older People Recognizing Depression in Older People Recognizing Depression in Older People Recognizing Depression in Older People Recognizing Depression in Older People Recognizing Depression in Older People
After discovering that your loved one has been diagnosed with Alzheimer’s or dementia, you may have a series of questions about adjusting to day-to-day life. Are they safe? Does my loved one understand what’s going on? How do I communicate with them? All are valid and pressing questions that our knowledgeable team can address. How can the right environment help someone with dementia?
When it comes to in-home safety, there are specific precautions and needed changes to make your environment safe. Dr. Piero Antuono, Silverado Brookfield Medical Director says the living environment plays a crucial role on the lifestyle for a person with dementia. Take in regard a living space that minimizes anxiety and noise, which can also additionally reduce feelings of anxiety, depression, confusion, and isolation.
We’ve also gathered some essential safety tips from Silverado in-home care experts. See if your living environment makes the cut.
- Register a Bracelet
The MedicAlert + Alzheimer’s Association Safe Return program is available for individuals with dementia who may wander off, in which case the registered bracelet will have personalized information such as emergency contacts and health history. The bracelet is registered with local law enforcement to ensure that your loved one will be returned home safely. You can register an individual online through the Alzheimer’s Association. - Install Motion Detectors
Some motion detectors today have video capabilities, and some even have responsive automated voices. Experts suggests installing devices around the house, which helps to have another set of eyes to watch your loved one from wherever you are. - Remove rugs
As they are the number one cause of falls in the home, removing all rugs from teh home can be an important step to make the environment safer. - Take No Solicitors
Consider posting a “No Solicitors” sign at the front door to avoid any unexpected visitors. Also, have other family members pick up the phone, because a person with dementia can often be the victim of telephone exploitation. Keep the phone ringer volume on low and make everyone in the household aware that the phone should be answered in as few rings as possible. This will avoid possible distraction and confusion. - Remove Locks
Consider removing locks from the bathroom in case your loved one locks themselves inside. - Emergency Contacts
Display emergency numbers in every room and next to all telephones. - Lighting
Be sure lighting around the house is adequate, including entryways, corners, hallways, bathrooms, stairs, and outside landscaping. Lights with sensors may also be useful. - Electronics
Prevent fire hazards by keeping electronics on sturdy surfaces, covering unused electrical outlets and clearing any extension cords, which also minimizes the likelihood of trips and falls. - Prevent Slips
Install handles and grab bars around the house as safety grips. The handrail for stairways should extend beyond the first and last steps. To prevent slips, use nonskid adhesives in the tub, toilets, and sinks.
For more videos of dementia specialists answering common questions click here.
How can the right environment help someone with dementia?
How can the right environment help someone with dementia? How can the right environment help someone with dementia? How can the right environment help someone with dementia? How can the right environment help someone with dementia?How can the right environment help someone with dementia?
10 Reasons To Work With An Independent Timeshare Consultant
- You’ve “Googled” timeshare and come up with 15 million responses. Need a little help editing those responses?
- 2. How do you know which of the thousands of timeshares on the resale market is the best fit for your needs?
- How many timeshare sales pitches have you gone on? Do you know the “timeshare movie” by heart?
- Hmmm, the timeshare salesperson started by saying that the price was $40,000…by the time the manager came over, the price dropped down to $10,000. Did you find that confusing?
- Did you really believe the last timeshare salesperson you dealt with…the 22 year old who said that he owned a 3-bedroom in Hawaii?
- What does “all red, all the time” really mean?
- You get the price of just about everything else online, why won’t the developer give you the price of the timeshare online?
- You’re confused with all the media coverage about timeshare being a lousy investment. Isn’t spending money on hotel bills a lousy investment?
- Why would you buy anything after listening to a biased salesperson for 2 hours? Do you buy anything else that way?
- How many more “cheap” timeshares do you want to buy before you realize “cheap” isn’t necessarily good?
Lisa Ann Schreier has been involved in the timeshare community since 1998. After cutting her teeth as a timeshare salesperson and manager at a number of Orlando area resorts, she grew increasingly frustrated with the antiquated marketing and high pressure sales techniques that were (and sadly still are) the norm in the industry. Seeking to be a catalyst for positive change, she wrote ‘Surviving A Timeshare Presentation…Confessions From The Sales Table’ and ‘Timeshare Vacations For Dummies.’ She is a frequent contributor to major media outlets and a sought after speaker at consumer advocacy groups. In addition to her articles at Senior.com, she is the lead timeshare advocate at Elliott.org and a featured blogger on RockStarFinance.com. Her ‘tell it like it is’ blog about timeshare issues is a source of solid information and continues to alert consumers to the myriad of less than reputable companies and practices.
Lisa’s blog can be accessed at: http://www.thetimesharecrusader.blogspot.com
Twitter users can follow her at @LisaLooksAt
Questions? Looking for assistance? Email Lisa at lisaschreier617@gmail.com
10 Reasons To Work With An Independent Timeshare Consultant 10 Reasons To Work With An Independent Timeshare Consultant 10 Reasons To Work With An Independent Timeshare Consultant 10 Reasons To Work With An Independent Timeshare Consultant 10 Reasons To Work With An Independent Timeshare Consultant 10 Reasons To Work With An Independent Timeshare Consultant 10 Reasons To Work With An Independent Timeshare Consultant
Because massage relaxes the muscles and calms the mind, it can provide a variety of benefits for people suffering from physical and mental ailments. Due to the number of physical complications that accompany Diabetes, as well as the emotional stress of coping with the disease, massage therapy has been shown to alleviate certain types of Diabetic complications. How Massage Chairs Help People with Diabetes
According to the American Diabetes Association, an estimated 1 out of 3 Diabetics over the age of 50 will suffer from Peripheral Arterial Disease (PAD). PAD occurs when the blood vessels in the legs are narrowed and blocked by fatty deposits, and the blood flow to the feet is decreased. This can result in an alarming number of consequences ranging from foot ulcers to amputation. Therefore, it is critical for Diabetics to ensure that the blood flow to their legs is regulated.
Massage products—from recliners with foot-and-calf massagers, to targeted foot-and-calf relief solutions—can serve as an incredibly useful tool for people seeking to increase blood flow in their legs and feet. The Figure-Eight Technology® in many Human Touch® products deliver an advanced massage technique that emulates those used by a professional masseuse, and increases the blood flow between the legs and torso.
Massage has been shown to drop glucose levels, which can help to prevent Hyperglycemia in Diabetics. According to Healthline.com, Hyperglycemia can cause eye damage, cardiovascular disease, kidney failure, nerve damage (Neuropathy), skin and gum infections, joint problems, and can even result in a diabetic coma. Helping to relax your body with massage will assist in lowering your glucose levels, which can prevent these types of Hyperglycemic ailments.
Another benefit of massage for Diabetics is the increase in flexibility as the muscles are loosened through massage. High blood sugar can result in the thickening of connective tissue, and massage will increase the mobility and elasticity of that tissue. As the muscles, tendons, and ligaments are relaxed, massage recipients will find an increase in motion and flexibility in the joints, therefore improving their quality of life.
Important Precautions
All of these benefits of massage should be noted by anyone suffering from the symptoms of Diabetes. However, there are a few important factors to consider when seeking massage therapy.
As with any type of physical therapy, it is critical to consult with your physician before commencing. Massage is a great option for anyone seeking stress and pain relief, but Diabetics will need to be aware that the fluxuations in their blood sugar levels need careful observation at all times. The delicate balance of their insulin injections and glucose levels must be monitored, and reduced glucose may influence the amount of insulin they require.
It is also important to avoid massage in an area where Diabetics inject their insulin. Pressure in this area may influence the way that their body absorbs the shot, and therefore alter their intake.
As a final recommendation, Diabetics who suffer from Neuropathy should be cautious when assessing the pressure levels and heat options from any massage service, whether from a masseuse or a massage chair. Due to the nerve damage associated with Neuropathy, it may be difficult to determine the appropriate massage intensity or heat levels that work for their body, and misuse can result in bruising or overheated skin. It is recommended for those with Neuropathy to consult with a professional, friend, or family member to determine if the massage technique or heating levels are ideal for a person of their body type and sensitivity levels.
Shop Massage Chairs
How Massage Chairs Help People with Diabetes
How Massage Chairs Help People with Diabetes How Massage Chairs Help People with Diabetes How Massage Chairs Help People with Diabetes How Massage Chairs Help People with Diabetes How Massage Chairs Help People with Diabetes How Massage Chairs Help People with Diabetes
How to Juggle Caregiver Tasks When You Work Outside the Home
According to the National Caregiver Alliance and AARP, 60% of the approximately 43.5 million caregivers in the U.S. are employed, and most of them work outside the home full time. Balancing Caregiving Responsibilities and Work
Between work, caregiving tasks and maintaining their own household, it’s no wonder the majority of caregivers report that they experience physical and emotional stress. Between work and caregiving, they are putting in at least 60 hours a week!
Shortcuts to Balance the Caregiver/Employee Roles
If you’re not able to cut back work or caregiving hours, how can you balance the two? Shortcuts, hacks and letting things go is a good start. Here are my best timesavers and hacks that I’ve used during extremely stressful and busy times.
1. Eat as well as I can:
I’d love to say, hey, get your 5 servings of vegetables and fruits in every day, but let’s face it, when you’re busy, the easiest food to eat is usually junk food or processed food. When I’m super busy, I try to make sure we’re stocked with portable healthy snacks such as granola bars, string cheese, yogurt, bananas, tangerines and apples. Aside from the yogurt and cheese, I can throw them in my bag or leave them in my car. Balancing Caregiving Responsibilities and Work
2. Cook in bulk:
It isn’t the most exciting way to eat, but I usually cook two or three large meals at the beginning of the week and we re-heat throughout the week.
3. Sunday or Monday plan:
I once read an article about a woman who keeps her Mondays appointment free so that she could prepare herself for a successful week. Monday doesn’t work for most people who have a full-time job, but for me, Sunday evening is a great time to plan for the week. Balancing Caregiving Responsibilities and Work
I personally prefer a paper calendar for planning, although I keep an electronic calendar so that I have it on my phone as well. For planning, I look at both and go through the days of the week and make sure we are covered for any appointments and activities. I bought a dry erase decal for my refrigerator that I use for any appointments that affect more than one person so my husband and I are on the same page.
If you are scheduling yourself and your parent, you may want to color code your schedule. One thing that tripped up a lot of my clients and their children was backing up times to allow for transportation. There were many times where they would accidentally leave for an appointment at the time they were supposed to arrive. One of my clients who was an executive assistant in her career had a great idea of putting her pick up time in pen and underneath, she would write the appointment time in pencil. I am hooked on these Bic four color pens since I can easily color-code without having to have multiple pens. They last forever. I have been using the same one for 2 years now. Balancing Caregiving Responsibilities and Work
4. Schedule maintenance:
If you are so busy that you are barely getting through the day, making sure the little things continue to run is important, but challenging. Go ahead and put your car maintenance on your calendar ahead of time so that you don’t forget. The last thing you need is an expensive car repair. Are there other things you need to maintain? Think about what needs to be done to keep your life running smoothly and put it on your calendar before you forget – both for your home and your parent. Balancing Caregiving Responsibilities and Work
5. Maximize your work day:
If you have to be in an office for eight hours a day, use your lunch or breaks to get some tasks done. During your planning time, list out any appointments you need to make (with phone numbers and any background info), shop for groceries online and do any other task that you don’t need to do in person. If you have your list and all the details ready to go, you can blaze through your list. Balancing Caregiving Responsibilities and Work
If you don’t sit at a desk or don’t work at a computer, you can still take your lunch break to make any calls, set up appointments, etc. You can also shop on Amazon Prime Now from your cell phone.
6. Find off-hour service providers:
While most doctors only operate from 9 a.m. – 5 p.m., there are some dentists and even medical imaging centers that are open late or on weekends. I once had an MRI at 9 a.m. on a Saturday. Try to find providers that operate when you have more time for you and your parent so that you don’t need to use all of your time off for routine care.
7. Get creative:
I worked with a family who had a creative strategy for medical appointments. They hired us to transport the father to and from his appointment, but the daughter met him there, attended the appointment and went back to work. She only needed to take one hour off of work, versus 3 hours if she was providing transportation.
Can you find ways to be present without doing everything? Can you schedule appointments early in the morning so that you only miss an hour of work. Is there someone you can split the load with? Do you have a friend, neighbor or community member who has more free time and can assist with some of the manageable tasks like grocery shopping or errands? Is there someone you can hire to help with the errands? I haven’t tried it yet, but I’ve heard of sites like Task Rabbit, where you can hire someone to do errands for you. Balancing Caregiving Responsibilities and Work
You can’t do it all, so finding shortcuts or getting help can help take some of the stress off your plate. How can you find a few extra hours? Balancing Caregiving Responsibilities and Work
Balancing Caregiving Responsibilities and Work
According to the latest estimates from the World Health Organization (WHO), more than 300 million people worldwide live with depression. These estimates make depression the leading cause of ill health and disability at a global scale. The number of people with depression increased by more than 18% between 2005 and 2015. 6 Ways for Seniors to Beat Depression
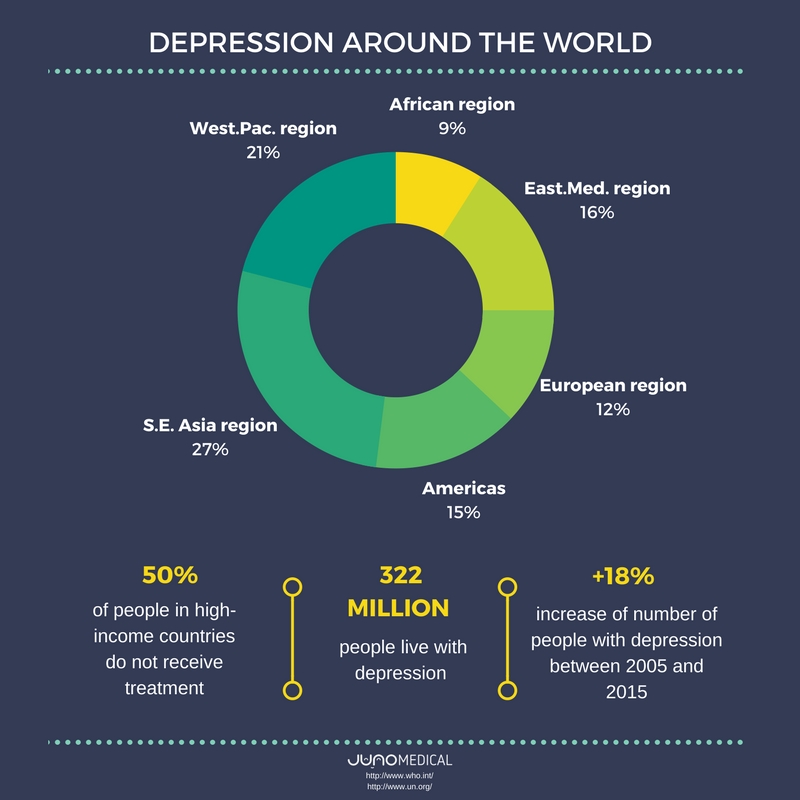
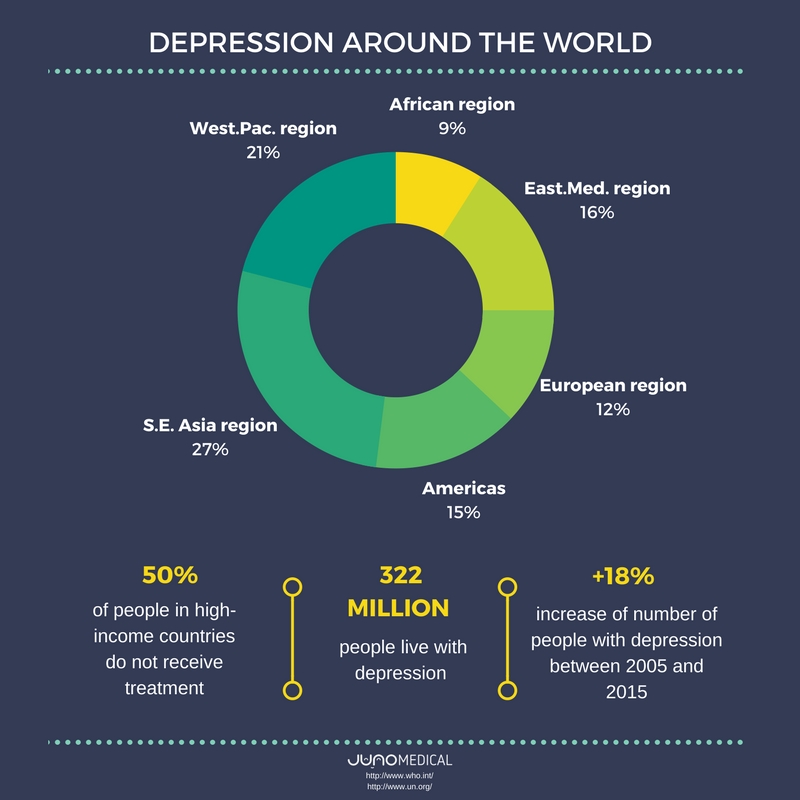
Depression around the world according to regions, as specified in the infographic:
| Region | Percentage |
|---|---|
| African region | 9% |
| Eastern Mediterranean region | 16% |
| European region | 12% |
| South-East Asia region | 27% |
| Region of the Americas | 15% |
| Western Pacific region | 21% |
Nearly 50% of these people live in the South-East Asia region and Western Pacific region, reflecting the relatively larger populations of those two regions (which include India and China, for example).
In order to raise awareness, the 2017 World Health Day (April 7th) will focus on depression. To this aim, the WHO has organized a year-long campaign, Depression: let’s talk.
In terms of support available for people with mental health disorders, the need of increased investments is clear. Even in high-income countries, nearly 50% of people with depression do not get treatment. On average, just 3% of government health budgets is invested in mental health, varying from less than 1% in low-income countries to 5% in high-income countries.
How is depression affecting the elderly?
Depressive disorders involve sadness, loss of interest or pleasure, feelings of tiredness, disturbed sleep or appetite, feelings of guilt or low self- worth, and poor concentration. Depression impairs the ability of an individual to function at work or school and cope with daily life.
In terms of age groups, prevalence peaks in older adulthood (above 7.5% among females aged 55-74 years, and above 5.5% among males).
This striking number has encouraged us to focus on depression in the elderly, as it is often overlooked and untreated.
There are various factors that can lead to depression as a consequence of life changes that come with aging.
“One thing that is vital to understand when dealing with depression in older adults is that they are often having to deal with loss,” says Louise Morse, cognitive behavioral therapist at Pilgrims’ Friend Society. “Loss of physical and mental agility, perhaps, but always loss of family members, both older ones (who passed away) and younger ones (who moved away for work). The combination of losses can be overwhelming. They lose people who help reflect back to them their identity: people they can bounce things off and trust, people with whom they have shared memories”.
- loss of interest in activities that they would normally enjoy and inability to carry out daily activities, for at least two weeks
- loss of energy, change in appetite; different sleeping patterns; anxiety; reduced concentration; restlessness; feelings of worthlessness, guilt, or hopelessness; and thoughts of self-harm or suicide.
- depression among older people is often associated with physical conditions, such as heart disease, high blood pressure, or diabetes. Life events, such as losing a partner; and a reduced ability to do things that were possible when younger, may also contribute to depression.
Depression is treatable, with talking therapies or antidepressant medication or a combination of these.
How can you help?
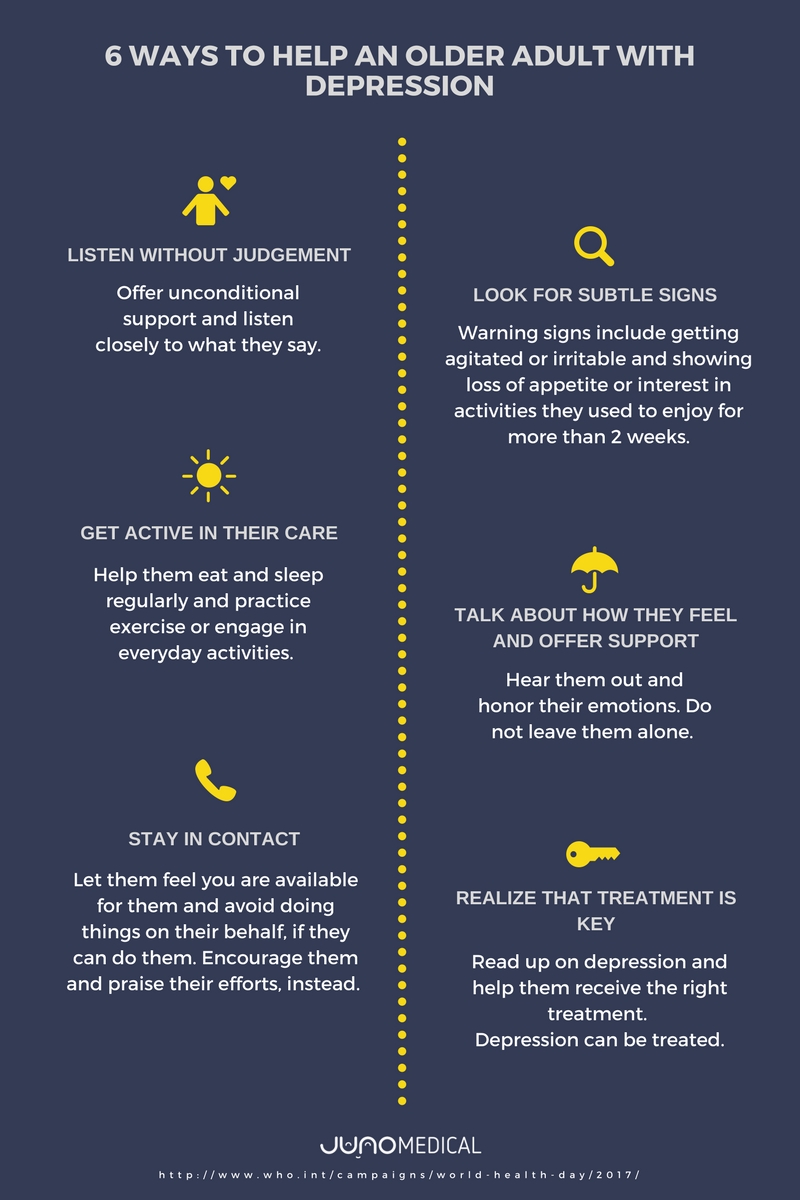
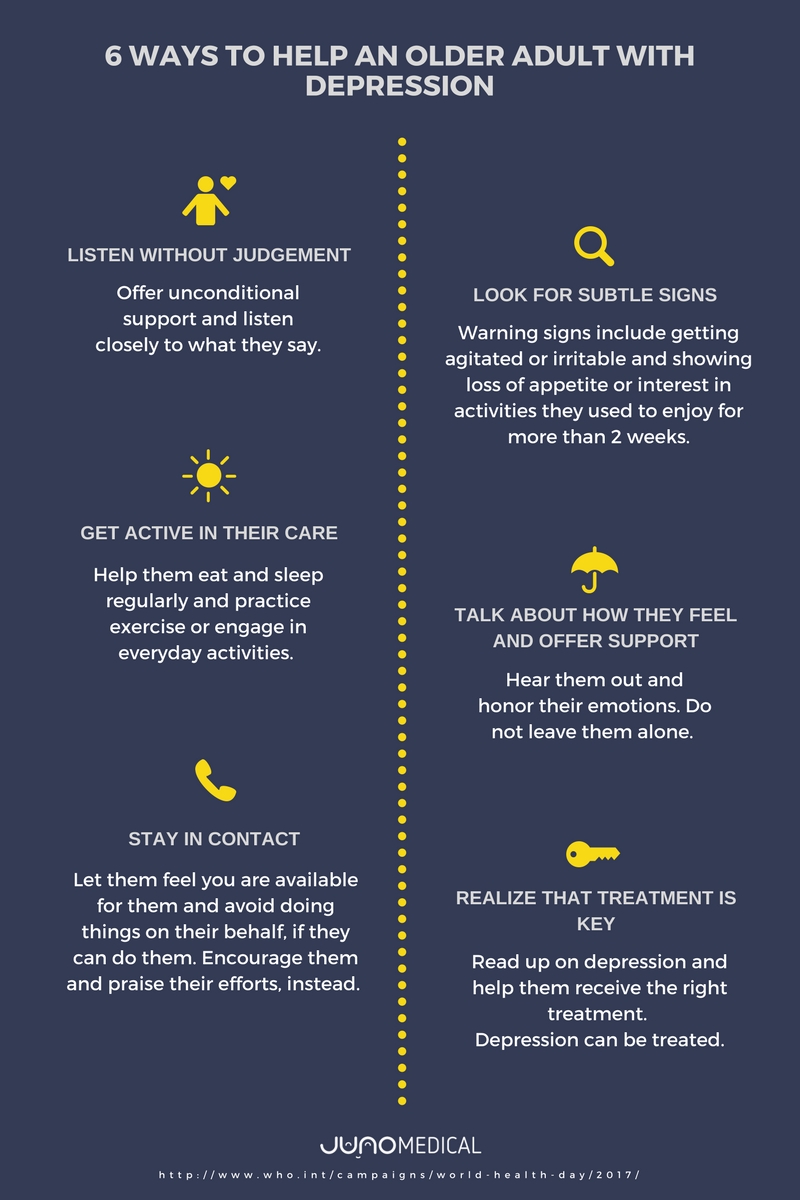
1. Listen without judgment
Offer unconditional support and listen closely to what the person says: little or subtle changes in their life can be warning signs.
2. Look for subtle signs
Read up on and get a clear understanding of depression. Signs of distress may involve wringing hands excessively, getting agitated or irritable, or having difficulty sitting still. Older adults often do not say they feel sad or lonely because they don’t want to be a burden on the family. Other possible signs include loss of appetite or interest in activities that they used to enjoy for more than two weeks.
3. Get active in their care
Go to appointments together and if any medication is prescribed, help your elderly relative to take them. Help them have a regular eating and sleeping pattern and encourage them to undertake everyday activities and practice exercise.
4. Talk about how they feel and offer support
It’s really important to hear them out and honor their emotions. The elderly are often less likely to cope with loss or difficult life events. “One thing that could really help is to go over some of their memories and walk through their landscape. They can feel very isolated at times”, says Louise Morse.
5. Realize that treatment is key
Depression can be treated. Family members should be aware of the disability that depression can cause and should offer their support in receiving the right treatment.
6. Stay in contact
Let the person feel you are available for them. At the same time, don’t take care over their life and do things that they can do for themselves. It would only reinforce their perception that they are worthless and incapable. Instead, help them break tasks into steps and praise them for any efforts.
Another great article: “When you feel lonely”
By JunoMedical
www.junomedical.com
For more information about depression:
World Health Organization (WHO): http://www.who.int/topics/depression/en/
Anxiety and Depression Association of America: https://www.adaa.org/
American Psychological Association: http://www.apa.org/topics/depression/
European Depression Association: http://eddas.eu/
6 Ways for Seniors to Beat Depression
6 Ways for Seniors to Beat Depression 6 Ways for Seniors to Beat Depression 6 Ways for Seniors to Beat Depression 6 Ways for Seniors to Beat Depression 6 Ways for Seniors to Beat Depression 6 Ways for Seniors to Beat Depression 6 Ways for Seniors to Beat Depression 6 Ways for Seniors to Beat Depression 6 Ways for Seniors to Beat Depression 6 Ways for Seniors to Beat Depression 6 Ways for Seniors to Beat Depression 6 Ways for Seniors to Beat Depression
Depression In Older Adults Depression In Older Adults Depression In Older Adults Depression In Older Adults
Why Seniors Should Consider Rehab an Option
Contrary to popular belief, addiction is not just an affliction of the young. More than 1 million adults ages 65 and older in this country have a substance use disorder, according to 2017 data from the Substance Abuse and Mental Health Services Administration (SAMHSA). This number is projected to rise, with a vast majority of affected seniors never seeking treatment in what has been aptly termed “a growing, but mostly silent, epidemic” in a 2016 study from BMC Health Services Research. Am I Too Old for Drug or Alcohol Rehab?
Sadly, what many older people with addiction don’t know is that rehab is both a viable and promising option for kicking a drug or alcohol problem. Seniority should never be an obstacle to getting effective treatment for an addiction.
Why Older Adults Should Go to Rehab
First, consider these three compelling reasons to go to rehab for a drug or alcohol problem.
- Older adults have better rates of recovery.
A 2013 Hazelden reportsheds light on why this is so. Recovery rates in seniors are higher than those in younger people because “older adults have more positive experiences to draw upon and tend to be more disciplined about recovery.”
Another key predictor of success in recovery is a client’s adherence to a plan of drug or alcohol treatment. When researchers in a 2002 studycompared older clients’ adherence to alcohol treatment with younger clients’ adherence to alcohol treatment, they found the older clients were more likely to comply with their plan of treatment. They were more faithful about attending therapy sessions and taking prescribed medications. As a result, the older adults’ rates of relapse were lower than those among younger adults.
- Drugs and alcohol are more physically harmful in older age.
There are a number of reasons that a drug or alcohol problem that you may have successfully managed earlier in life is increasingly more dangerous to your health as you age. These include:
- A changing metabolism that raises your risks of a drug or alcohol-related fall or injury.
- An age-associated decline in your immune system, cognition and other physical functions.
- Your need for more over-the-counter medicines and doctor prescriptions as you age, accompanied by a greater likelihood of harmful interactions.
- Decreased mobility and social interactions that can feed your sense of isolation and contribute to more severe substance abuse and addiction
- There is no better time than now (the “Golden Years”) to improve your quality of life.
Contrary to the ageist mindset that says you’re too old to benefit from rehab, seniority is a persuasive reason to put quality-of-life concerns first. The golden years are an opportunity to make the most of the time you have left. Researchshows that people who attend inpatient rehab achieve a significant improvement in their quality of life.
For older people, moreover, positive and supportive relationships— not finances— are reportedly a more important quality-of-life measure. Strikingly, there is an even greater body of research that describes how treatment for addiction can improve close relationships with family and friends.
Tips for Finding the Right Rehab Program
Seniors who pursue treatment for an addiction have a number of rehab programs to choose from. Some cater exclusively to seniors, such as a nursing home that integrates addiction treatment into post-hospital rehab.
But don’t rule out a mixed-age rehab program either. Findings from the 2002 study cited above suggested that individualized, age-appropriate psychotherapies are more important to a successful recovery than a seniors-only treatment setting.
Here are some other things to keep in mind when you’re looking for a rehab program:
- Detox time– Detox typically takes longer in older adults, so look for a program that will provide you with a medically supervised withdrawal that is safe and complete.
- Dual diagnosis program– Substance abuse in older adults can often co-occur with symptoms of anxiety or depression related to grief, loss of mobility and/or other life transitions that come with age. Look for programs that are “dual diagnosis” (meaning they treat both substance use and co-occurring disorders).
- Customized therapies for your psychosocial needs– Similarly, substance abuse typically has psychosocial and emotional roots that need to be addressed. Among older adults, these may relate to issues like depression or complicated or unresolved grief. Ask about what sorts of therapies will be offered to address these sorts of issues, and to what extent these therapies will be provided on an individual basis.
- Location of program– If you have age-related health and mobility issues, you may wish to stay closer to home for rehab. Alternatively, if you’re able to travel, a program that is out of state may provide you with more of a retreat-like experience.
- The tone of the staff towards older adults– Try to gauge whether there is a tone of positive support, respect and care for older adult clients. Pay attention to how the staff responds to your requests and inquiries when you call or tour the facility. If you pick up on any age-related condescension, that’s an immediate red flag.
- Length of treatment– No matter your age group, you’ll experience better recovery outcomes the longer you stay in treatment, so ask about the length of the program.
No older adult should forego treatment because of concerns about their age. If you’re young enough to drink or use drugs, you’re young enough for rehab. Period.
By Anna Ciulla
Anna Ciulla is the Vice President of Clinical and Medical Services at Beach House Center for Recovery, where she oversees the supervision and delivery of client care. Anna has an extensive background in psychotherapy and clinical management and is often invited to speak and write for various audiences on issues related to addiction. She writes on a variety of addiction and recovery-related topics, including the benefits of seeking treatment no matter your age or place in life.
Support Systems for Elderly Dealing with Substance Abuse
Am I Too Old for Drug or Alcohol Rehab?
Am I Too Old for Drug or Alcohol Rehab? Am I Too Old for Drug or Alcohol Rehab? Am I Too Old for Drug or Alcohol Rehab? Am I Too Old for Drug or Alcohol Rehab? Am I Too Old for Drug or Alcohol Rehab? Am I Too Old for Drug or Alcohol Rehab? Am I Too Old for Drug or Alcohol Rehab? Am I Too Old for Drug or Alcohol Rehab? Am I Too Old for Drug or Alcohol Rehab? Am I Too Old for Drug or Alcohol Rehab? Am I Too Old for Drug or Alcohol Rehab? Am I Too Old for Drug or Alcohol Rehab?
Industry Experts Weigh in on Medical Services that Beneficiaries thought Medicare Paid for that Don’t
New Medicare beneficiaries tend to assume they’re fully covered by Original Medicare benefits. Unaware of the gaps in coverage, they end up finding out the hard way when they receive a medical bill in the mail. Industry Experts Explain What Medicare Actually Covers
Medicare Parts A & B only covers 80% of your medical costs. It has no out of pocket maximum and no prescription drug coverage. If you, or someone you know, only has Original Medicare, then this article pertains to you. Below, you’ll learn from industry experts as they explain what Medicare covers.
Medicare Does Not Cover it all
“We hear from many people who assume that long term care is covered by Medicare. Most are caught by surprise by that fact that Medicare does not cover long term care, only short-term rehab. This usually comes up when a loved one is no longer able to return home after a hospital stay and the shocking reality of paying privately for a care option is upon them. Another area we hear about Medicare not covering is scooters and walk-in tubs. These items are rarely covered by Medicare and once again, people are surprised by this harsh reality.” Amie Clark – Co-Founder of TheSeniorlist.com
- Medicare does not cover Long-term care or support for your personal care needs. Most long-term care is not medical care, it is help with activities of daily living or personal tasks of everyday life. Medicare does suggest visiting LongTermCare.gov for information and resources to help you plan your long-term care needs. Medicare does cover care in a long-term care hospital, skilled nursing care in a skilled nursing facility, eligible home health services, hospice and respite care. Medicare will help cover durable medical equipment (DME) like scooters, walkers and wheelchairs if you have a medical need and qualify.
“People often assume that long term care, such as that provided by a nursing home, or a home health aide, is covered by Medicare. Unfortunately, that is not the case. Medicare will only pay for some short-term services after a hospitalization. Long term care can become a massive financial burden for much of the elderly population in the United States.” – Rebecca Gilbert, MD, PhD, APDA Vice President, Chief Scientific Officer.
- Long term care not being covered can be a burden on beneficiaries and their families. I would recommend getting long-term care insurance before it is needed or too late. Many people are uninsured or underinsured, talking to an Insurance Agent to get questions answered and find the right plan for you is the best thing you can do.
“Patients and physicians are frequently confused about personal care services covered under Medicare benefits. They do not understand the difference between skilled and non-skilled home care services. For example, Medicare benefits cover a home health CNA when there is a skilled need and the patient meets home health criteria, including homebound status. Receiving this home health CNA service is temporary and can only be offered while nursing and/or therapy services are being provided, and at a low frequency (e.g. 1-2 visits per week). Non-skilled personal care services are not covered by insurance at this time and are paid privately or through special waivers. There is no time limit or guidelines as to who can receive personal care services since they are paid privately. Furthermore, DME supplies, such as transfer benches, adaptive feeding equipment and braces, are thought to be covered by Medicare, but are not. This is needed for safety in the home and should be covered to reduce further decline.” Sarah Deal – Interim Healthcare Inc
- Having affordable DME supplies is vital for the elderly and disabled. While there are some DME supplies covered by Medicare, there are strict standards and both the doctor and the DME supplier need to accept Medicare assignment.
“There are several medical services that are not covered by Medicare that can cause a problem for seniors and their families. Many people have the preconceived misconception that Medicare pays for everything. On the contrary, there are Medicare deductibles, coinsurance and copays that has spawned a whole industry of supplemental plans to fill in the Medicare “gaps”. One of the areas that is not covered by Medicare is long-term care. We see this as a surprise to people on Medicare and their families because it is an area of care that so many seniors rely on later in life. However, Medicare itself does not cover nursing homes or custodial care. Now, there are insurance plans that you can purchase to cover that type of care, but these would, ideally, need to be purchased well before those benefits are needed. Another medical service that is not covered by “original” Medicare is prescription drugs. Prescription drug coverage for Medicare beneficiaries is provided through Medicare Part D. This is always a separate plan, sold through a private company, and it must be signed up for separately (you are not automatically enrolled in prescription drug coverage in most situations). Also, if you delay enrollment into prescription drug Part D coverage, you may face higher premiums due to Medicare’s Part D late enrollment penalty. Other medical care that is non-covered by Medicare are services for routine hearing, vision and dental care. There are some related aspects of these services that are covered, such as cataract surgery for example. But overall, routine care is not covered for hearing, vision or dental – this includes hearing aids, eyeglasses, and fillings, extractions, crowns, etc. You can purchase insurance to cover these things, but Medicare itself does not cover them.” Garrett Ball – Medicare Specialist at Senior.com
- Medicare is not the most comprehensive coverage available. It does not cover many services. It is important for the Medicare beneficiary to purchase additional coverage. Some plans will include routine hearing, vision, and dental care. Part D Prescriptions Drug plans will need to be purchased through a private insurance company and you can be penalized if you are not enrolled in one when your part B goes into effect. Medicare is not the only insurance you want when something goes wrong with your health, you need to purchase additional coverage.
What you Can do to Prevent being Underinsured
Medicare does not cover everything; especially not long-term (custodial) care, routine dental, vision, hearing or prescription drugs. Working with an Insurance Agent or Counselor will help you get the coverage you need so you will be properly insured. Choose a plan that allows you to have the most consistent and reliable coverage year after year.
Looking for affordable DME products? Senior.com is a leader in the industry with affordable pricing and great customer service.
dustry Experts Explain What Medicare Actually Covers
Industry Experts Explain What Medicare Actually Covers Industry Experts Explain What Medicare Actually Covers Industry Experts Explain What Medicare Actually Covers Industry Experts Explain What Medicare Actually Covers Industry Experts Explain What Medicare Actually Covers Industry Experts Explain What Medicare Actually Covers Industry Experts Explain What Medicare Actually Covers Industry Experts Explain What Medicare Actually Covers Industry Experts Explain What Medicare Actually Covers Industry Experts Explain What Medicare Actually Covers Industry Experts Explain What Medicare Actually Covers
Is Your Aging Parent Struggling?
Whether you live near your aging parents or live across the country, it can be hard to see changes in their health or well-being. Sometimes, health and cognitive changes are gradual, making it hard to notice. Or, in many cases, we just see our parents as our parents and don’t notice a decline until something major happens. Signs Your Aging Parent Needs Caregiving Support
It can be especially hard for local family members to see gradual changes. Similar to noticing gradual weight loss in someone you see regularly, you may not catch that your parent has lost interest in activities or that they seem to more and more forgetful. Sometimes, it takes an extended visit from a long-distance family member to catch these changes.
I worked with many families who had both long-distance and local siblings. It was always interesting to see how much more the long-distance siblings noticed, since they had more time between visits so changes to health and wellbeing seemed more drastic, rather than gradual. Many times, I noticed issues that local family members didn’t see since they weren’t looking for signs of illness or decline.
I had a client who had two daughters who were not on the same page about his well-being. The local sister saw nothing wrong with her father’s balance and gait because he had been walking like that for some time. The sister who visits a few times a year from Spain was shocked by how much her father had declined and insisted on a life alert system and that his driving service walk him to his apartment, rather than leave him in the garage, which was his preference. My staff and I knew that he struggled and had brought it up to the local daughter but she dismissed us, until her sister expressed the same concern.
Signs Your Aging Parent is Struggling
Here are some changes you should keep an eye out for, whether you live nearby or across the country.
- Depression: While depression can be common in older adults, there are ways to combat depression. If you notice slight changes such as a loss of interest in activities they previously enjoyed or feelings of guilt, consider addressing these concerns with your parent or their physician.
- Increase in Falls: Is your aging parent falling more frequently? If you’ve already addressed fall risks in the home, it could be due to a medical condition or their medication. Speak with their doctor and consider fall prevention aides.
- Loneliness: Has your parent recently lost a close friend, moved away from their neighborhood or stopped driving? They could be lonely, which can lead to physical and emotional health problems.
- Unsafe Driving: Are you noticing new dings or dents on your parents’ car? Are they anxious about getting behind the wheel? Do they have limited mobility or hearing loss? These could be signs that they need to turn over the keys. Help them understand the dangers of unsafe driving and find solutions to keep them independent and active.
- Elder Abuse: Is there someone who is getting abnormally close to your loved one or who is trying to keep family members away from your parent? They may be committing elder abuse. Trust your gut and get informed. Elder abuse isn’t just physical abuse.
- Malnutrition: Did you know that many seniors suffer from malnutrition? Help your parents remain proper nutrition by stocking them up with easy healthy snacks and ensuring healthy meals are accessible to them.
- Alzheimer’s Disease: Are you noticing your parent isn’t just forgetting little details, but significant facts such as how to get home from the grocery store or trouble following simple directions? There is a difference between general cognitive decline and dementia. Don’t ignore the signs. Signs Your Aging Parent Needs Caregiving Support
Don’t dismiss changes to health and well-being. With some tweaks or discussions with a doctor, they can probably be rectified, but if you let something like malnutrition or financial fraud go on for too long, it can have a catastrophic effect.
Signs Your Aging Parent Needs Caregiving Support
Signs Your Aging Parent Needs Caregiving Support
Signs Your Aging Parent Needs Caregiving Support Signs Your Aging Parent Needs Caregiving Support Signs Your Aging Parent Needs Caregiving Support Signs Your Aging Parent Needs Caregiving Support










